Conditions & Symptoms
We are dedicated and focused on pain relief of the back and neck, both acute or chronic.
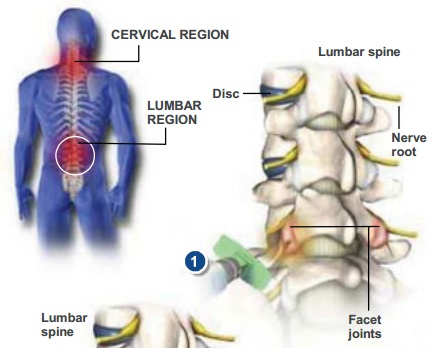
Epidural Anesthetic Block & Steroid Injection
Epidural Nerve Blocks Cervical / Thoracic / Lumbar
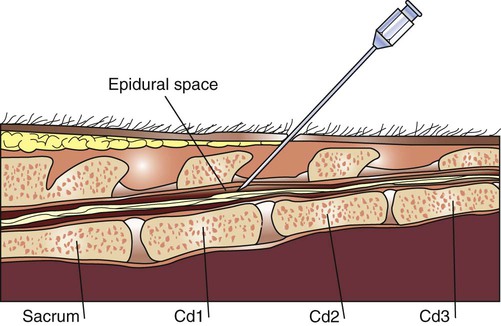 A block that is performed under fluoroscopy to confirm a specific diagnosis and/or decrease pain and inflammation.
A block that is performed under fluoroscopy to confirm a specific diagnosis and/or decrease pain and inflammation.
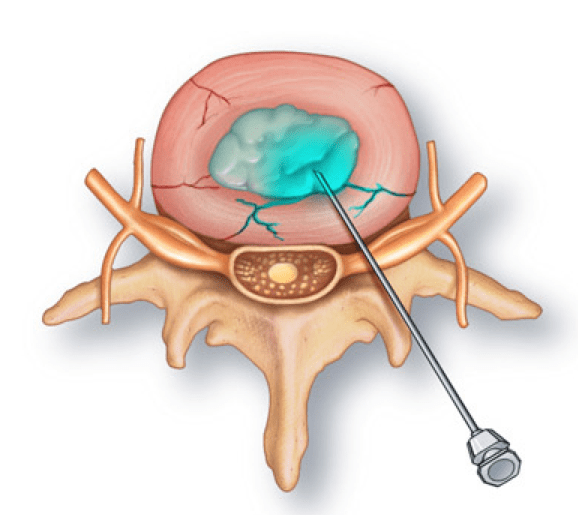
A local skin anesthetic is given. A special needle is then inserted into the epidural space of the Cervical, Thoracic, lumbar or caudal spine. Fluoroscopy is used to guide the needle and prevent complications from the needle. Contrast medium is injected into the space to confirm proper placement and outline the effect of the herniation on the spine and nerve roots, films are taken for review with the patient. An anesthetic and then a steroid (usually a long acting- slow release type of cortisone) are injected into the epidural space.
Relief of pain if the medication reaches the inflamed area or source of pain.
Fifteen minutes plus approximately fifteen to forty-five minutes recovery time depending or not as to whether sedation is given.
 An epidural steroid injection is performed to help reduce the inflammation and pain associated with nerve root compression. Nerve roots can be compressed by a herniated disc, spinal stenosis, and bone spurs. When the nerve is compressed it becomes inflamed. This can lead to pain, numbness, tingling or weakness along the course of the nerve. This is called radiculopathy. The goal of the epidural steroid injection is to help lessen the inflammation of the nerve root. The epidural space is located above the outer layer surrounding the spinal cord and nerve roots. An epidural steroid injection goes into the epidural space, directly over the compressed nerve root.
An epidural steroid injection is performed to help reduce the inflammation and pain associated with nerve root compression. Nerve roots can be compressed by a herniated disc, spinal stenosis, and bone spurs. When the nerve is compressed it becomes inflamed. This can lead to pain, numbness, tingling or weakness along the course of the nerve. This is called radiculopathy. The goal of the epidural steroid injection is to help lessen the inflammation of the nerve root. The epidural space is located above the outer layer surrounding the spinal cord and nerve roots. An epidural steroid injection goes into the epidural space, directly over the compressed nerve root.
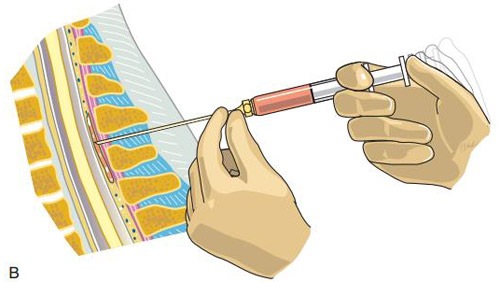
Kyphoplasty
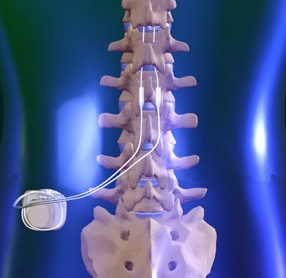
Spinal Cord Stimulator Trial, Implatn, and Management
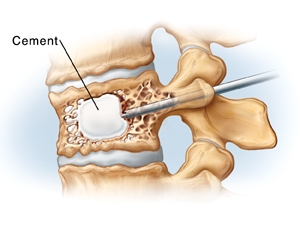
A medical procedure that is similar to vertebroplasty in the use of acrylic cement to stabilize and reduce pain associated with a vertebral compression fracture but that additionally restores vertebral height and lessens spinal deformity by injecting the cement into a cavity created in the fractured bone by the insertion and inflation of a special balloon.
A medical procedure that is similar to vertebroplasty in the use of acrylic cement to stabilize and reduce pain associated with a vertebral compression fracture but that additionally restores vertebral height and lessens spinal deformity by injecting the cement into a cavity created in the fractured bone by the insertion and inflation of a special balloon.

MILD is a safe procedure that can help patients diagnosed with lumbar spinal stenosis (LSS) stand longer and walk farther with less pain. It is a short, outpatient procedure, performed through a very small incision (about the size of a baby aspirin) that requires no general anesthesia, no implants, and no stitches.

Morphine pump implantation is a surgical procedure performed to permanently implant a pump that delivers morphine to the spinal fluid to treat chronic pain.
What is its goal?
The aim of the operation is to implant a pump that will deliver morphine to the spinal fluid for the treatment and relief of pain. This sometimes avoids some of the side effects encountered with very high doses of narcotic pain medication like morphine.
How is it done?
During a pre-operative trial, morphine is injected into the spinal canal (using a small needle) and you are assessed by the treatment team over several hours to determine how well the medicine treats the pain. If a positive effect is observed then you may be a candidate for implantation of a permanent pump to delver the drug.
The pump is inserted under the covering of the abdominal muscles while the patient is under a general anesthetic. A small catheter is then inserted through a needle into the spinal fluid space and is threaded upward. The catheter is then tunneled under the skin to the abdomen and is connected to the pump. The pump is filled with the drug morphine and is programmed by a computer to continuously release a specified dose that is determined by the physician.
The operation is completed when the incision is closed with suture material (stitches) or surgical staples. If the outer incision is closed with staples or non-absorbable sutures, they will have to be removed after the incision has healed. The procedure usually lasts 1-2 hours.
What are the risks?
There are always risks with any surgery. Potential complications may include:
- Pain, numbness, weakness or paralysis due to nerve damage (rare)
- Cerebrospinal fluid leak
- Recurrence or continuation of pain.
- Bleeding/injury to blood vessels
- Infections
- General anesthetic complications
Hardware related complications during surgery is rare but can include catheter migration. After surgery though, the potential hardware complications include: catheter fracture or migration, infection or pump malfunction.
What is the success rate?
The success rate of morphine pump implantation for delivery of morphine to the spinal fluid is generally favorable. Patients tend to have had a good response with their pain control in pre-operative trials. This is the permanent implantation phase.
How long will I stay in the hospital?
After the surgery, patients are in the hospital for a few days. Each individual patient’s return to normal activity is largely dependent on his/her pre-operative condition and age. Typically you will be able to go home once your vital signs are stable, you can walk on your own, you can eat without having nausea, and you have resumed normal bladder activity. Follow-up will be needed as the pump will need to be refilled every couple of months, depending on the pump size, concentration and dose. Refills are done in the office using a syringe and needle and take approximately fifteen minutes to complete. At that time, morphine doses are adjusted depending on the effects that are being seen.
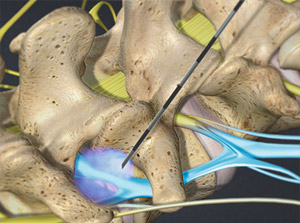
Also known as a zygapophysial joint block, the facet joint block is performed to determine whether a facet joint is a source of pain. Facet joints are located on the back of the spine, where one vertebra slightly overlaps another. These joints guide and restrict the spines movement.
A facet joint injection is a precise diagnostic tool that also provides excellent therapeutic results. Using fluoroscopic (x-ray) guidance, physicians are able to see and accurately target the affected joint(s). Facet joints are the small joints located between each vertebra that provide the spine with both stability and flexibility. Facet syndrome occurs when one or more of these joints become inflamed or irritated. Arthritis occurs when the cartilage lining the joint surface shrinks and wears thin, causing stress on the bone (bone spurs), inflammation, and enlargement of the joint.
Facet joint injections combine a local anesthetic and a corticosteroid anti-inflammatory medication. This mixture relieves both pain and inflammation coming from the involved joint. A successful result supports the diagnosis that the facet joint is indeed the “pain generator” and the cause of your back pain. Because they are performed using local anesthetic, facet joint injections offer the advantage of providing immediate feedback in confirming the source of your pain.
How Long does Each Procedure Take?
Both of these procedures are safely performed on an outpatient basis. Facet joint injections take 20 to 30 minutes. Radiofrequency neurotomy takes 30 to 60 minutes, depending on the number of levels that require treatment. Each of these procedures is followed by approximately 45 minutes of observed recovery time.
How Often can these Procedures be Done?
Facet joint injections are generally limited to three within a six-month time frame. In many instances, only one or two injections are required to obtain benefit. Radiofrequency neurotomy or denervation is usually effective after one treatment. Radiofrequency may be repeated every one to two years, if necessary.
What are the Expected Results?
Facet joint injections have been performed safely for many years with very positive outcomes. In the hours following the procedure, however, you may have a sore back or neck for one to two days. It’s recommended that you take it easy the day of the procedure, but return to your usual activities the following day. The pain relief benefits from facet joint injections typically begin on the second to third day.
With radiofrequency neurotomy, most patients begin noting improvement within two weeks. Successful radiofrequency neurotomy typically provides relief for nine to fourteen months, and for some patients up to two years and beyond. These treatment approaches offer significant pain resolution without the potential risks and down time of surgery.
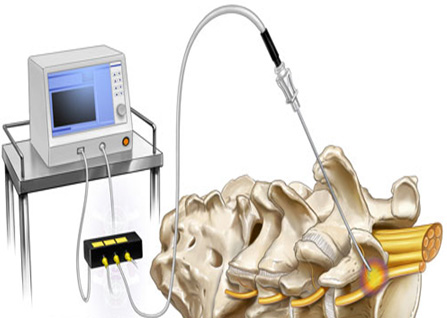
What is a radiofrequency neuroablation?
A radiofrequency neuroablation is a minimal invasive procedure that reduces pain that orientating from the facets joints of your neck or spine.
How does a radiofrequency neuroablation work?
Heat is used to cauterize specific nerves to interfere temporarily with their ability to send pain signals to the brain. The radiofrequency neuroablation procedure is typically performed after you have demonstrated pain relief from a “test” injection such as a medial branch block.
How is a radiofrequency neuroablation performed?
An experienced pain physician will use a needle-like tube called a cannula and positions it into the irritated medial branch nerve area using x-ray or fluoroscopic guidance to ensure treatment accuracy. Once the physician has verified positioning, the radiofrequency electrode is inserted through the cannula. The physical will test the position of the cannula by sending a weak electrical jolt to the nerve. If the weak electric jolt increases the pain without any muscle effects, the electrode is positioned correctly. The physician proceeds use the electrode to cauterize the nerve and this blocks the pain signal from being sent to the brain. The procedure typically takes 60 minutes or less, and patients can leave shortly after their procedure is complete.
How long will the relief last for?
Many patients report pain relief up to one year or more.
How often can I have a radiofrequency neuroablation?
Since nerves grow back, repeating the procedure is necessary. In many instances patients will have the procedure repeated every 12-18 months.
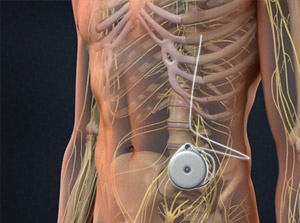
A spinal infusion pump implant, commonly known as a morphine pump, is a specialized device which delivers concentrated amounts of medication into the spinal fluid space via a small catheter. The intrathecal space is the sac that contains the spinal fluid. The spinal infusion pump is also known as an intrathecal infusion pump.
A transforaminal or selective nerve root block is an injection of local anesthetic and steroid injected under x-ray guidance into the area where the nerve exits the spinal column. A block is usually ordered by your doctor for pain in the arm or leg that follows the path of a single nerve. This block may be diagnostic and/or therapeutic. One of three things may happen. 1. The pain does not go away – which means that the pain is probably not coming from the nerve at the level of the injection – this has diagnostic value. 2. The pain goes away and stays away for a few hours but the original pain comes back and doesn’t get better again. This would mean the block was also of diagnostic value – the pain is probably coming from the nerve at the level of the injection, but the steroid was not of benefit. 3. The pain goes away after the block, the pain may come back later that day, but then the pain gets better again over the next few days.
Risks of the procedure
As with most procedures there is a remote risk of bleeding, infection, nerve injury, or allergic reaction to the medications used. Some short-term side effects may occur. You should get some numbness that follows the path of the nerve that was blocked. You may get some weakness as well. If you get weakness that interferes with your ability to walk, you will have to remain in the Ambulatory Surgery Center until this resolves – usually several hours. You may have increased pain for a few days after the injection, including localized pain at the injection site. Diabetics may have short-term elevation of blood sugars. People prone to fluid retention may have increased fluid retention for 1 – 2 weeks.
Most people say the stinging/burning of the numbing medicine is the most uncomfortable part of the procedure though every person’s response to any procedure is individual. As the injection is right near a nerve it is possible to get a temporary “electric-shock” sensation.
WHAT IS IT?
A block (or local anesthetic injection) that is performed to confirm that a facet joint is the source of pain and decrease pain and inflammation in a facet joint or joints.
Actually this is the only true way to diagnose facet joint syndrome, as an abnormal looking joint on x-ray or ct scan, may be painless, and vice versa a normal looking joint may be the pain generator.
HOW IS IT DONE?
The patient is given the option of light, (or deep in rare cases) iv sedation under monitoring of the ekg, pulse oximeter, etc by a board certified anesthesiologist. A tiny needle (smaller than the size of a paper clip) is then inserted into the area of the facet joint where the nerve reaches it (or directly inside the facet capsule, in some cases) and the physician injects an anesthetic and steroid.
This is done under fluoroscopy. I usually do the first one with a short acting local to quickly diagnose the levels of facet injury involved.
EXPECTED RESULTS?
Decrease in or relief of back pain. More importantly confirmation of the diagnosis, with the allowance of rational treatment.
HOW LONG DOES IT TAKE?
Fifteen to thirty minutes, depending on the number of levels performed.
Note: Injections may be done in conjunction with massage, myo-fascial release, or “light” physical therapy especially ultrasound and stimulation. Chiropractic will universally aggravate facet joint syndrome and must be avoided at all costs.
RISK / BENEFIT RATIO:
Probably the easiest of all interventional procedures (provided done by a board certified physician with experience), with the lowest risk and most benefits.
OTHER THERAPY:
Once, the diagnosis is made by a prognostic block, the block may be repeated with a longer acting local and depot steroid preparation. Some milder cases may be treated, by improving posture, spine bracing during lifting/exercise and anti-arthritic agents such as motrin or the newer (cox-2) inhibitors such as celebrex or vioxx. If the pain recurs, pulsed radiofrequency is the definitive treatment (see inside).
FACET JOINT SYNDROME (Definition):
A constellation of symptoms which result in diffuse pains that do not fit a clear nerve root pattern (e.g. Not sciatica), these pains are worsened with movement of the spine, poor posture, often sleep, sometimes associated with cold burning sensations, usually worsened by cold damp weather and are now known to emanate from the tiny medial branch nerves that supply the facet joint.
Remember the only way to definitively make the diagnosis is by a diagnostic/prognostic facet block.
Discography confirms or denies the disc(s) as a source of your pain. It is a relatively simple procedure that uses a small needle to inject contrast dye into your disc. MRI and CT scans only demonstrate anatomy and cannot absolutely prove your pain source. In many instances, discs are abnormal on MRI or CT scans but are not a source of pain. Only discography, which is a functional test, can tell if the disc itself is a source of your pain. Discography is usually done only if you think your pain is significant enough for you to consider more advanced treatment options, directed at the disc itself, such as surgery.
